Singapore researchers develop bandage that can wirelessly assess wounds
Last Updated on December 30, 2022 by Admin
[ad_1]
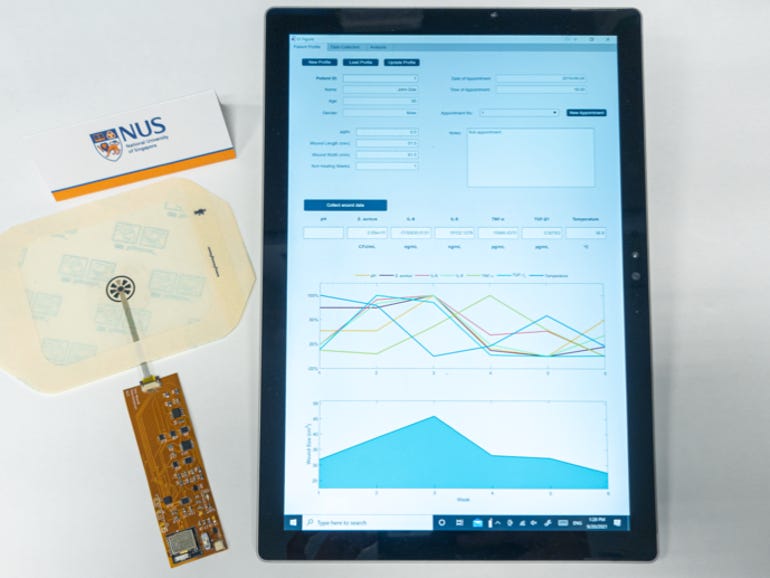
(Credit: National University of Singapore)
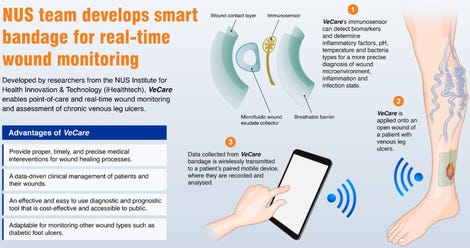
Researchers in Singapore say they have developed a bandage that can detect and wirelessly send medical information related to chronic wounds, such as temperature and bacteria type. With the ability to capture and transmit such data in under 15 minutes, the wearable sensor is touted to speed up assessment of such wounds and provide more timely treatment.
Called VeCare, the platform encompasses a “wound sensing bandage”, an electronic chip, and a mobile app through which data is transmitted, said the research team from the Department of Biomedical Engineering and Institute for Health Innovation & Technology (iHealthtech) at National University of Singapore (NUS). The researchers also worked with clinical partners from Singapore General Hospital (SGH).
The bandage features a wound contact layer, breathable outer barrier, microfluidic fluid collector, and a flexible immunosensor, NUS said in a statement Thursday. Using an electrochemical system, the bandage detect various biomarkers specific to chronic wounds and facilitate the assessment of the wound’s microenvironment, inflammation, and state of infection.
The microfluidic wound fluid collector, which is attached to the sensor, directs and enhances fluid delivery to the sensor by up to 180%, according to NUS, adding that this helps ensure the sensor can perform reliably regardless of the ulcer shape or size.
The microchip also is embedded with flexible electronics connected to the sensor, enabling data to be transmitted wirelessly to the app for on-site assessment and analysis in real-time. Data is sent to the patient’s paired mobile device, on which it is stored and analysed. This processor also is powered by a rechargeable battery.
Collectively, the VeCare wearable sensor system can detect temperature, acidity, bacteria type, and inflammatory factors specific to chronic wounds. Its ability to do so within 15 minutes would facilitate timely and accurate assessment of such wounds, which was critical to a patient’s recovery, NUS said.
It said clinical tests were carried out with SGH involving patients with chronic venous leg ulcers, which the university said “successfully demonstrated” the platform’s effectiveness in assessing and monitoring such wounds.
Faced with an ageing population, Singapore was seeing more patients with non-healing wounds such as diabetic foot and chronic venous leg ulcers.
NUS noted that the healing process of chronic wounds often were disrupted due to various reasons, including infections and repeated trauma, and could lead to more severe outcomes such as foot amputation for sufferers of diabetic foot ulcers. Ensuring timely medical care and treatment, while essential, required multiple and lengthy visits to clinics and would drive up healthcare costs.
For one, clinical assessments of wounds currently depended on visual inspection or collection of wound fluid, which then had to be sent to a centralised lab for analysis of specific biomarkers. This process typically took one to two days.
The VeCare system system was designed to address such challenges as well as enable doctors to monitor the patient’s condition remotely, reducing the need for patients to travel to a clinic.
NUS’ iHealthtech director Lim Chwee Teck, who led the research team, said: “Point-of-care devices coupled with telehealth or digital health capability can play a significant role in transforming the healthcare industry and our society, which is catalysed by the COVID-19 pandemic requirements for safe distancing. Our smart bandage technology is…designed for chronic wound management to give patients the freedom to perform the test and monitor their wound conditions at home.”
Lim said VeCare could be customised to monitor different panels of biomarkers and various types of wounds.
“The aim is to have an effective and easy to use diagnostic and prognostic tool for precise and data-driven clinical management of patients,” he added.
The research team now was focused on further developing VeCare to meet safety and regulatory requirements as well as for mass production, NUS said.
Another research team from the university in June said it developed a way to tap the human body as a medium to draw energy and power wearables. The technology enabled power to be extracted from a single device, such as a mobile phone placed in a pocket, to wirelessly charge other wearables placed on the body. It also could be used to pull unused energy from electronic appliances in homes or offices to power wearables.
RELATED COVERAGE
[ad_2]
Source link




